Monday, 28 March 2016
Can Blue-Colored Light Prevent Suicide?
An intriguing, anecdotal finding was recently reported by some news outlets that the implementation of blue-colored streetlights has reduced both crime and suicides:
Glasgow, Scotland, introduced blue street lighting to improve the city’s landscape in 2000. Afterward, the number of crimes in areas illuminated in blue noticeably decreased.Since the railway company introduced the new blue lights, they’ve had no new suicide attempts.
The Nara, Japan, prefectural police set up blue street lights in the prefecture in 2005, and found the number of crimes decreased by about 9 percent in blue-illuminated neighborhoods. Many other areas nationwide have followed suit.
Keihin Electric Express Railway Co. changed the color of eight lights on the ends of platforms at Gumyoji Station in Yokohama, Japan, in February.
This effect may be attributed to a few possible reasons (some of which are mentioned in the comments section of the article):
- The light color is new and unusual, causing people to act more cautiously in the area (as a person is unsure what to expect in the unusually-lit area).
- Blue is a light color almost universally associated with a police presence, suggesting it is an area of stricter law enforcement.
- Blue may be a more pleasant illuminating color to most people, as opposed to yellow, orange or red (according to some research, such as Lewinski, 1938).
Prof. Tsuneo Suzuki at Keio University said: “There are a number of pieces of data to prove blue has a calming effect upon people. However, it’s an unusual color for lighting, so people may just feel like avoiding standing out by committing crimes or suicide under such unusual illumination. It’s a little risky to believe that the color of lighting can prevent anything.”There is a lot of research into the psychology of color, but not as much has looked into the color of blue illumination itself (as opposed to the color of an object or wall). But some research looking into short wavelength light (blue) has demonstrated that it is a potentially effective treatment for seasonal affective disorder (a seasonal type of depression; see for instance, Glickman, et al., 2006), and helps to reduce the stress response in fish (it hasn’t been yet tested on humans).
If this finding is robust and the behavior change associated with it is still prevalent a few years from now (when everyone has become accustomed to the new light color), it would be an interesting finding. A simple, inexpensive change might be effective in helping reduce at least one method of suicide (and reduce crime to boot).
Sunday, 27 March 2016
Acute stress reaction
"Acute stress response" was first described by Walter Cannon in the 1920s as a theory that animals react to threats with a general discharge of the sympathetic nervous system.
The response was later recognized as the first stage of a general
adaptation syndrome that regulates stress responses among vertebrates
and other organisms.
The onset of a stress response is associated with specific physiological actions in the sympathetic nervous system, both directly and indirectly through the release of adrenaline and to a lesser extent noradrenaline from the medulla of the adrenal glands. These catecholamine hormones facilitate immediate physical reactions by triggering increases in heart rate and breathing, constricting blood vessels. An abundance of catecholamines at neuroreceptor sites facilitates reliance on spontaneous or intuitive behaviors often related to combat or escape.
Normally, when a person is in a serene, unstimulated state, the "firing" of neurons in the locus ceruleus is minimal. A novel stimulus, once perceived, is relayed from the sensory cortex of the brain through the thalamus to the brain stem. That route of signaling increases the rate of noradrenergic activity in the locus ceruleus, and the person becomes alert and attentive to the environment.
If a stimulus is perceived as a threat, a more intense and prolonged discharge of the locus ceruleus activates the sympathetic division of the autonomic nervous system (Thase & Howland, 1995). The activation of the sympathetic nervous system leads to the release of norepinephrine from nerve endings acting on the heart, blood vessels, respiratory centers, and other sites. The ensuing physiological changes constitute a major part of the acute stress response. The other major player in the acute stress response is the hypothalamic-pituitary-adrenal axis.
If symptoms last for more than a month, then the patient might be instead diagnosed with PTSD.
Studies have been conducted to assess the efficacy of counselling and psychotherapy for people with ASD. Cognitive behavioral therapy which included exposure and cognitive restructuring was found to be effective in preventing PTSD in patients diagnosed with ASD with clinically significant results at 6 months follow-up. A combination of relaxation, cognitive restructuring, imaginal exposure, and in vivo exposure was superior to supportive counseling.[4] Mindfulness based stress reduction programs also appear to be effective for stress management.[5]
Signs and symptoms
Common symptoms that sufferers of acute stress disorder experience are: numbing; emotional detachment; muteness; derealization; depersonalization; psychogenic amnesia; continued re-experiencing of the event via thoughts, dreams, and flashbacks; and avoidance of any stimulation that reminds them of the event. During this time, they must have symptoms of anxiety, and significant impairment in at least one essential area of functioning. Symptoms last for a minimum of 2 days, and a maximum of 4 weeks, and occur within 4 weeks of the event.Causes
Acute stress disorder (abbreviated ASD, and not to be confused with autism spectrum disorder) is the result of a traumatic event in which the person experiences or witnesses an event that causes the victim/witness to experience extreme, disturbing, or unexpected fear, stress, or pain, and that involves or threatens serious injury, perceived serious injury, or death to themselves or someone else. A study of rescue personnel after exposure to a traumatic event showed no gender difference in acute stress reaction. [1] Acute stress reaction is a variation of post-traumatic stress disorder (PTSD).The onset of a stress response is associated with specific physiological actions in the sympathetic nervous system, both directly and indirectly through the release of adrenaline and to a lesser extent noradrenaline from the medulla of the adrenal glands. These catecholamine hormones facilitate immediate physical reactions by triggering increases in heart rate and breathing, constricting blood vessels. An abundance of catecholamines at neuroreceptor sites facilitates reliance on spontaneous or intuitive behaviors often related to combat or escape.
Normally, when a person is in a serene, unstimulated state, the "firing" of neurons in the locus ceruleus is minimal. A novel stimulus, once perceived, is relayed from the sensory cortex of the brain through the thalamus to the brain stem. That route of signaling increases the rate of noradrenergic activity in the locus ceruleus, and the person becomes alert and attentive to the environment.
If a stimulus is perceived as a threat, a more intense and prolonged discharge of the locus ceruleus activates the sympathetic division of the autonomic nervous system (Thase & Howland, 1995). The activation of the sympathetic nervous system leads to the release of norepinephrine from nerve endings acting on the heart, blood vessels, respiratory centers, and other sites. The ensuing physiological changes constitute a major part of the acute stress response. The other major player in the acute stress response is the hypothalamic-pituitary-adrenal axis.
Diagnosis
There must be a clear temporal connection between the impact of an exceptional stressor and the onset of symptoms; onset is usually within a few minutes or days but may occur up to one month after the stressor. In addition, the symptoms show a mixed and usually changing picture; in addition to the initial state of "daze," depression, anxiety, anger, despair, overactivity, and withdrawal may all be seen, but no one type of symptom predominates for long; the symptoms usually resolve rapidly in those cases where removal from the stressful environment is possible; in cases where the stress continues or cannot by its nature be reversed, the symptoms usually begin to diminish after 24–48 hours and are usually minimal after about 3 days.[2]If symptoms last for more than a month, then the patient might be instead diagnosed with PTSD.
Treatment
This disorder may resolve itself with time or may develop into a more severe disorder such as PTSD. However, results of Creamer, O'Donnell, and Pattison's (2004) study of 363 patients suggests that a diagnoses of acute stress disorder had only limited predictive validity for PTSD. Creamer et al. did find that re-experiences of the traumatic event and arousal were better predictors of PTSD.[3] Medication can be used for a short duration (up to four weeks).[citation needed]Studies have been conducted to assess the efficacy of counselling and psychotherapy for people with ASD. Cognitive behavioral therapy which included exposure and cognitive restructuring was found to be effective in preventing PTSD in patients diagnosed with ASD with clinically significant results at 6 months follow-up. A combination of relaxation, cognitive restructuring, imaginal exposure, and in vivo exposure was superior to supportive counseling.[4] Mindfulness based stress reduction programs also appear to be effective for stress management.[5]
Alzheimer's disease
Alzheimer's disease (AD), also known as Alzheimer disease, or just Alzheimer's, accounts for 60% to 70% of cases of dementia.[1][2] It is a chronic neurodegenerative disease that usually starts slowly and gets worse over time.[1][2] The most common early symptom is difficulty in remembering recent events (short-term memory loss).[1] As the disease advances, symptoms can include problems with language, disorientation (including easily getting lost), mood swings, loss of motivation, not managing self care, and behavioural issues.[1][2] As a person's condition declines, they often withdraw from family and society.[1] Gradually, bodily functions are lost, ultimately leading to death.[3] Although the speed of progression can vary, the average life expectancy following diagnosis is three to nine years.[4][5]
The cause of Alzheimer's disease is poorly understood.[1] About 70% of the risk is believed to be genetic with many genes usually involved.[6] Other risk factors include a history of head injuries, depression, or hypertension.[1] The disease process is associated with plaques and tangles in the brain.[6] A probable diagnosis is based on the history of the illness and cognitive testing with medical imaging and blood tests to rule out other possible causes.[7] Initial symptoms are often mistaken for normal ageing.[1] Examination of brain tissue is needed for a definite diagnosis.[6] Mental and physical exercise, and avoiding obesity may decrease the risk of AD.[6] There are no medications or supplements that decrease risk.[8]
No treatments stop or reverse its progression, though some may temporarily improve symptoms.[2] Affected people increasingly rely on others for assistance, often placing a burden on the caregiver; the pressures can include social, psychological, physical, and economic elements.[9] Exercise programmes are beneficial with respect to activities of daily living and can potentially improve outcomes.[10] Treatment of behavioural problems or psychosis due to dementia with antipsychotics is common but not usually recommended due to there often being little benefit and an increased risk of early death.[11][12]
In 2015, there were approximately 48 million people worldwide with AD.[2] It most often begins in people over 65 years of age, although 4% to 5% of cases are early-onset Alzheimer's which begin before this.[13] It affects about 6% of people 65 years and older.[1] In 2010, dementia resulted in about 486,000 deaths.[14] It was first described by, and later named after, German psychiatrist and pathologist Alois Alzheimer in 1906.[15] In developed countries, AD is one of the most financially costly diseases.[16][17]
At present, there is no definitive evidence to support that any particular measure is effective in preventing AD.[117]
Global studies of measures to prevent or delay the onset of AD have
often produced inconsistent results. Epidemiological studies have
proposed relationships between certain modifiable factors, such as diet,
cardiovascular risk, pharmaceutical products, or intellectual
activities among others, and a population's likelihood of developing AD.
Only further research, including clinical trials, will reveal whether
these factors can help to prevent AD.[118]
Long-term usage of non-steroidal anti-inflammatory drugs (NSAIDs) is associated with a reduced likelihood of developing AD.[124] Evidence also support the notion that NSAIDs can reduce inflammation related to amyloid plaques.[124] No prevention trial has been completed.[124] They do not appear to be useful as a treatment.[125] Hormone replacement therapy, although previously used, may increase the risk of dementia.[126]
Conclusions on dietary components have at times been difficult to ascertain as results have differed between population-based studies and randomised controlled trials.[130] There is limited evidence that light to moderate use of alcohol, particularly red wine, is associated with lower risk of AD.[134] There is tentative evidence that caffeine may be protective.[135] A number of foods high in flavonoids such as cocoa, red wine, and tea may decrease the risk of AD.[136][137]
Reviews on the use of vitamins and minerals have not found enough consistent evidence to recommend them. This includes vitamin A,[138][139] C,[140][141] E,[141][142] selenium,[143] zinc,[144] and folic acid with or without vitamin B12.[145] Additionally vitamin E is associated with health risks.[141] Trials examining folic acid (B9) and other B vitamins failed to show any significant association with cognitive decline.[146] In those already affected with AD adding docosahexaenoic acid, an omega-3 fatty acid, to the diet has not been found to slow decline.[147]
Curcumin as of 2010 has not shown benefit in people even though there is tentative evidence in animals.[148] There is inconsistent and unconvincing evidence that ginkgo has any positive effect on cognitive impairment and dementia.[149] As of 2008 there is no concrete evidence that cannabinoids are effective in improving the symptoms of AD or dementia.[150] Some research in its early stages however looks promising.[151]
The cause of Alzheimer's disease is poorly understood.[1] About 70% of the risk is believed to be genetic with many genes usually involved.[6] Other risk factors include a history of head injuries, depression, or hypertension.[1] The disease process is associated with plaques and tangles in the brain.[6] A probable diagnosis is based on the history of the illness and cognitive testing with medical imaging and blood tests to rule out other possible causes.[7] Initial symptoms are often mistaken for normal ageing.[1] Examination of brain tissue is needed for a definite diagnosis.[6] Mental and physical exercise, and avoiding obesity may decrease the risk of AD.[6] There are no medications or supplements that decrease risk.[8]
No treatments stop or reverse its progression, though some may temporarily improve symptoms.[2] Affected people increasingly rely on others for assistance, often placing a burden on the caregiver; the pressures can include social, psychological, physical, and economic elements.[9] Exercise programmes are beneficial with respect to activities of daily living and can potentially improve outcomes.[10] Treatment of behavioural problems or psychosis due to dementia with antipsychotics is common but not usually recommended due to there often being little benefit and an increased risk of early death.[11][12]
In 2015, there were approximately 48 million people worldwide with AD.[2] It most often begins in people over 65 years of age, although 4% to 5% of cases are early-onset Alzheimer's which begin before this.[13] It affects about 6% of people 65 years and older.[1] In 2010, dementia resulted in about 486,000 deaths.[14] It was first described by, and later named after, German psychiatrist and pathologist Alois Alzheimer in 1906.[15] In developed countries, AD is one of the most financially costly diseases.[16][17]
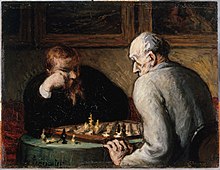
Prevention
Intellectual activities such as playing chess
or regular social interaction have been linked to a reduced risk of AD
in epidemiological studies, although no causal relationship has been
found.
Medication
Although cardiovascular risk factors, such as hypercholesterolaemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and course of AD,[119][120] statins, which are cholesterol lowering drugs, have not been effective in preventing or improving the course of the disease.[121][122][123]Long-term usage of non-steroidal anti-inflammatory drugs (NSAIDs) is associated with a reduced likelihood of developing AD.[124] Evidence also support the notion that NSAIDs can reduce inflammation related to amyloid plaques.[124] No prevention trial has been completed.[124] They do not appear to be useful as a treatment.[125] Hormone replacement therapy, although previously used, may increase the risk of dementia.[126]
Lifestyle
People who engage in intellectual activities such as reading, playing board games, completing crossword puzzles, playing musical instruments, or regular social interaction show a reduced risk for Alzheimer's disease.[127] This is compatible with the cognitive reserve theory, which states that some life experiences result in more efficient neural functioning providing the individual a cognitive reserve that delays the onset of dementia manifestations.[127] Education delays the onset of AD syndrome, but is not related to earlier death after diagnosis.[128] Learning a second language even later in life seems to delay getting Alzheimer disease.[129] Physical activity is also associated with a reduced risk of AD.[128]Diet
People who eat a healthy, Japanese, or Mediterranean diet have a lower risk of AD.[130] A Mediterranean diet may improve outcomes in those with the disease.[131] Those who eat a diet high in saturated fats and simple carbohydrates (mono- and disaccharide) have a higher risk.[132] The mediterranean diet's beneficial cardiovascular effect has been proposed as the mechanism of action.[133]Conclusions on dietary components have at times been difficult to ascertain as results have differed between population-based studies and randomised controlled trials.[130] There is limited evidence that light to moderate use of alcohol, particularly red wine, is associated with lower risk of AD.[134] There is tentative evidence that caffeine may be protective.[135] A number of foods high in flavonoids such as cocoa, red wine, and tea may decrease the risk of AD.[136][137]
Reviews on the use of vitamins and minerals have not found enough consistent evidence to recommend them. This includes vitamin A,[138][139] C,[140][141] E,[141][142] selenium,[143] zinc,[144] and folic acid with or without vitamin B12.[145] Additionally vitamin E is associated with health risks.[141] Trials examining folic acid (B9) and other B vitamins failed to show any significant association with cognitive decline.[146] In those already affected with AD adding docosahexaenoic acid, an omega-3 fatty acid, to the diet has not been found to slow decline.[147]
Curcumin as of 2010 has not shown benefit in people even though there is tentative evidence in animals.[148] There is inconsistent and unconvincing evidence that ginkgo has any positive effect on cognitive impairment and dementia.[149] As of 2008 there is no concrete evidence that cannabinoids are effective in improving the symptoms of AD or dementia.[150] Some research in its early stages however looks promising.[151]
Friday, 25 March 2016
Heart cancer
Heart cancer is an extremely rare form of cancer that is divided into primary tumors of the heart and secondary tumors of the heart.
Primary malignant cardiac tumors (PMCTs) are even more rare. A study using the Surveillance, Epidemiology and End-Results (SEER) Cancer Registry from 1973-2011 found 551 case of PMCTs, with an incidence of 34 cases per million persons. The study also found that the incidence has doubled over the past 4 decades. The associated mortality was very high, with only 46% of patients are alive by 1 year. Sarcomas and Mesotheliomas had the worst survival, while lymphomas had better survival. When compared with extracardiac tumors, PMCTs had worse survival. [3]
Primary
Most heart tumors begin with myxomas, fibromas, rhabdomyomas, and hamartomas, although malignant sarcomas (such as angiosarcoma or cardiac sarcoma) have been known to occur. In a study of 12,487 autopsies performed in Hong Kong seven cardiac tumors were found, most of which were benign.[1] According to Mayo Clinic: "At Mayo Clinic, on average only one case of heart cancer is seen each year."[1] In a study conducted in the Hospital of the Medical University of Vienna 113 primary cardiac tumour cases were identified in a time period of 15 years with 11 being malignant. The mean survival in the latter group of patients was found to be 26.2 ± 9.8 months.[2]Primary malignant cardiac tumors (PMCTs) are even more rare. A study using the Surveillance, Epidemiology and End-Results (SEER) Cancer Registry from 1973-2011 found 551 case of PMCTs, with an incidence of 34 cases per million persons. The study also found that the incidence has doubled over the past 4 decades. The associated mortality was very high, with only 46% of patients are alive by 1 year. Sarcomas and Mesotheliomas had the worst survival, while lymphomas had better survival. When compared with extracardiac tumors, PMCTs had worse survival. [3]
Atrial myxoma
An atrial myxoma is a benign tumor of the heart, commonly found within the left and right atria on the interatrial septum.
The tumor is derived from multipotential mesenchymal cells and may cause a ball valve-type obstruction.
About 75% of myxomas occur in the left atrium of the heart, usually beginning in the wall that divides the two upper chambers of the heart. The rest are in the right atrium. Right atrial myxomas are sometimes associated with tricuspid stenosis and atrial fibrillation.
Myxomas are more common in women. About 10% of myxomas are passed down through families (inherited). Such tumors are called familial myxomas. They tend to occur in more than one part of the heart at a time, and often cause symptoms at a younger age than other myxomas.
Right atrial myxomas rarely produce symptoms until they have grown to be at least 13 cm (about 5 inches) wide.
Tests may include:
Myxomas may come back if surgery did not remove all of the tumor cells.
Although a myxoma is not cancer, complications are common. Untreated, a myxoma can lead to an embolism (tumor cells breaking off and traveling with the bloodstream), which can block blood flow. Myxoma fragments can move to the brain, eye, or limbs.
If the tumor grows inside the heart, it can block blood flow through the mitral valve and cause symptoms of mitral stenosis. This may require emergency surgery to prevent sudden death.
Causes
Myxomas are the most common type of primary heart tumor.[1]The tumor is derived from multipotential mesenchymal cells and may cause a ball valve-type obstruction.
About 75% of myxomas occur in the left atrium of the heart, usually beginning in the wall that divides the two upper chambers of the heart. The rest are in the right atrium. Right atrial myxomas are sometimes associated with tricuspid stenosis and atrial fibrillation.
Myxomas are more common in women. About 10% of myxomas are passed down through families (inherited). Such tumors are called familial myxomas. They tend to occur in more than one part of the heart at a time, and often cause symptoms at a younger age than other myxomas.
Symptoms
Symptoms may occur at any time, but most often they accompany a change of body position. Symptoms may include:- Shortness of breath with activity
- Platypnea - Difficulty breathing in the upright position with relief in the supine position
- Paroxysmal nocturnal dyspnea - Breathing difficulty when asleep
- Dizziness
- Fainting
- Palpitations - Sensation of feeling your heart beat
- Chest pain or tightness
- Sudden Death (In which case the disease is an autopsy finding)
- Cough
- Fever
- Cachexia - Involuntary weight loss
- General discomfort (malaise)
- Joint pain
- Blue discoloration of the skin, especially the fingers (Raynaud's phenomenon)
- Fingers that change color upon pressure or with cold or stress
- Clubbing - Curvature of nails accompanied with soft tissue enlargement of the fingers
- Swelling - any part of the body
- Presystolic heart murmur[2]
Diagnosis
A doctor will listen to the heart with stethoscope. A "tumor plop" (a sound related to movement of the tumor), abnormal heart sounds, or a murmur similar to the mid-diastolic rumble of mitral stenosis may be heard. These sounds may change when the patient changes position.
Echocardiogram of Atrial myxoma
Tests may include:
- Echocardiogram and Doppler study
- Chest x-ray
- CT scan of chest
- Heart MRI
- Left heart angiography
- Right heart angiography
- ECG—may show atrial fibrillation
Treatment
The tumor must be surgically removed. Some patients will also need their mitral valve replaced. This can be done during the same surgery.Myxomas may come back if surgery did not remove all of the tumor cells.
Prognosis
An embolized fragment of an atrial myxoma in the iliac bifurcation.
If the tumor grows inside the heart, it can block blood flow through the mitral valve and cause symptoms of mitral stenosis. This may require emergency surgery to prevent sudden death.
Mediastinal tumor
The mediastinum is the cavity that separates the lungs from the rest of the chest. It contains the heart, esophagus, trachea, thymus, and aorta. The mediastinum has three main parts: the anterior mediastinum (front), the middle mediastinum, and the posterior mediastinum (back).
The most common mediastinal masses are neurogenic tumors (20% of mediastinal tumors), usually found in the posterior mediastinum, followed by thymoma (15-20%) located in the anterior mediastinum.[1]
Masses in the anterior portion of the mediastinum can include thymoma, lymphoma, pheochromocytoma, germ cell tumors including teratoma, thyroid tissue, and parathyroid lesions. Masses in this area are more likely to be malignant than those in other compartments.[2][3]
Masses in the posterior portion of the mediastinum tend to be neurogenic in origin, and in adults tend to be of neural sheath origin including neurilemomas and neurofibromas.[1]
Lung cancer typically spreads to the lymph nodes in the mediastinum.
In several editions of Physical Diagnosis,[4] concerning mediastinal tumors the author writes:
The most common mediastinal masses are neurogenic tumors (20% of mediastinal tumors), usually found in the posterior mediastinum, followed by thymoma (15-20%) located in the anterior mediastinum.[1]
Masses in the anterior portion of the mediastinum can include thymoma, lymphoma, pheochromocytoma, germ cell tumors including teratoma, thyroid tissue, and parathyroid lesions. Masses in this area are more likely to be malignant than those in other compartments.[2][3]
Masses in the posterior portion of the mediastinum tend to be neurogenic in origin, and in adults tend to be of neural sheath origin including neurilemomas and neurofibromas.[1]
Lung cancer typically spreads to the lymph nodes in the mediastinum.
In several editions of Physical Diagnosis,[4] concerning mediastinal tumors the author writes:
Diagnosis
According to Christian1 the mediastinal neoplasms which are neither so rare nor so obscure as to make diagnosis practically impossible are: (1) Sarcoma (including lymphosarcoma, leucaemic growths, and Hodgkins' disease; (2) Teratoma and cyst.
Thursday, 24 March 2016
Borderline personality disorder
Borderline personality disorder (BPD) is a pattern of abnormal behavior characterized by impulsivity, unstable affect, inconsistent interpersonal relationships, and poor self-image. Some individuals also display uncontrollable anger and depression. The pattern is typically present by early adulthood, and occurs across a variety of situations and contexts.[3] Other symptoms include intense fears of abandonment, sensitivity to feelings of rejection, and irritability of vague or uncertain origin.[3][4] People with BPD often engage in idealization and devaluation of others, alternating between high positive regard and great disappointment.[5] Self-harm, suicidal behavior, and substance abuse are commonly associated.[6]
The cause of BPD is unclear but believed to involve both genetic and environmental factors. A study done on twins suggested the illness could be inherited. Traits such as impulsiveness and aggression can be attributed to temperament.[7] There is evidence that abnormalities of the frontolimbic networks are associated with many of the symptoms.[8] The disorder is recognized in the Diagnostic and Statistical Manual of Mental Disorders. Since a personality disorder is a pervasive, enduring, and inflexible pattern of maladaptive inner experiences and pathological behavior, there is a general reluctance to diagnose personality disorders before adolescence or early adulthood.[9] However, some practitioners emphasize that without early treatment, the symptoms may worsen.[10]
There is an ongoing debate about the terminology of this disorder, especially the suitability of the word "borderline".[11][12] The ICD-10 manual refers to the disorder as emotionally unstable personality disorder and has similar diagnostic criteria. In the DSM-5, the name of the disorder remains the same as in the previous editions
The cause of BPD is unclear but believed to involve both genetic and environmental factors. A study done on twins suggested the illness could be inherited. Traits such as impulsiveness and aggression can be attributed to temperament.[7] There is evidence that abnormalities of the frontolimbic networks are associated with many of the symptoms.[8] The disorder is recognized in the Diagnostic and Statistical Manual of Mental Disorders. Since a personality disorder is a pervasive, enduring, and inflexible pattern of maladaptive inner experiences and pathological behavior, there is a general reluctance to diagnose personality disorders before adolescence or early adulthood.[9] However, some practitioners emphasize that without early treatment, the symptoms may worsen.[10]
There is an ongoing debate about the terminology of this disorder, especially the suitability of the word "borderline".[11][12] The ICD-10 manual refers to the disorder as emotionally unstable personality disorder and has similar diagnostic criteria. In the DSM-5, the name of the disorder remains the same as in the previous editions
Subscribe to:
Comments
(
Atom
)