Sunday, 27 March 2016
Alzheimer's disease
Alzheimer's disease (AD), also known as Alzheimer disease, or just Alzheimer's, accounts for 60% to 70% of cases of dementia.[1][2] It is a chronic neurodegenerative disease that usually starts slowly and gets worse over time.[1][2] The most common early symptom is difficulty in remembering recent events (short-term memory loss).[1] As the disease advances, symptoms can include problems with language, disorientation (including easily getting lost), mood swings, loss of motivation, not managing self care, and behavioural issues.[1][2] As a person's condition declines, they often withdraw from family and society.[1] Gradually, bodily functions are lost, ultimately leading to death.[3] Although the speed of progression can vary, the average life expectancy following diagnosis is three to nine years.[4][5]
The cause of Alzheimer's disease is poorly understood.[1] About 70% of the risk is believed to be genetic with many genes usually involved.[6] Other risk factors include a history of head injuries, depression, or hypertension.[1] The disease process is associated with plaques and tangles in the brain.[6] A probable diagnosis is based on the history of the illness and cognitive testing with medical imaging and blood tests to rule out other possible causes.[7] Initial symptoms are often mistaken for normal ageing.[1] Examination of brain tissue is needed for a definite diagnosis.[6] Mental and physical exercise, and avoiding obesity may decrease the risk of AD.[6] There are no medications or supplements that decrease risk.[8]
No treatments stop or reverse its progression, though some may temporarily improve symptoms.[2] Affected people increasingly rely on others for assistance, often placing a burden on the caregiver; the pressures can include social, psychological, physical, and economic elements.[9] Exercise programmes are beneficial with respect to activities of daily living and can potentially improve outcomes.[10] Treatment of behavioural problems or psychosis due to dementia with antipsychotics is common but not usually recommended due to there often being little benefit and an increased risk of early death.[11][12]
In 2015, there were approximately 48 million people worldwide with AD.[2] It most often begins in people over 65 years of age, although 4% to 5% of cases are early-onset Alzheimer's which begin before this.[13] It affects about 6% of people 65 years and older.[1] In 2010, dementia resulted in about 486,000 deaths.[14] It was first described by, and later named after, German psychiatrist and pathologist Alois Alzheimer in 1906.[15] In developed countries, AD is one of the most financially costly diseases.[16][17]
At present, there is no definitive evidence to support that any particular measure is effective in preventing AD.[117]
Global studies of measures to prevent or delay the onset of AD have
often produced inconsistent results. Epidemiological studies have
proposed relationships between certain modifiable factors, such as diet,
cardiovascular risk, pharmaceutical products, or intellectual
activities among others, and a population's likelihood of developing AD.
Only further research, including clinical trials, will reveal whether
these factors can help to prevent AD.[118]
Long-term usage of non-steroidal anti-inflammatory drugs (NSAIDs) is associated with a reduced likelihood of developing AD.[124] Evidence also support the notion that NSAIDs can reduce inflammation related to amyloid plaques.[124] No prevention trial has been completed.[124] They do not appear to be useful as a treatment.[125] Hormone replacement therapy, although previously used, may increase the risk of dementia.[126]
Conclusions on dietary components have at times been difficult to ascertain as results have differed between population-based studies and randomised controlled trials.[130] There is limited evidence that light to moderate use of alcohol, particularly red wine, is associated with lower risk of AD.[134] There is tentative evidence that caffeine may be protective.[135] A number of foods high in flavonoids such as cocoa, red wine, and tea may decrease the risk of AD.[136][137]
Reviews on the use of vitamins and minerals have not found enough consistent evidence to recommend them. This includes vitamin A,[138][139] C,[140][141] E,[141][142] selenium,[143] zinc,[144] and folic acid with or without vitamin B12.[145] Additionally vitamin E is associated with health risks.[141] Trials examining folic acid (B9) and other B vitamins failed to show any significant association with cognitive decline.[146] In those already affected with AD adding docosahexaenoic acid, an omega-3 fatty acid, to the diet has not been found to slow decline.[147]
Curcumin as of 2010 has not shown benefit in people even though there is tentative evidence in animals.[148] There is inconsistent and unconvincing evidence that ginkgo has any positive effect on cognitive impairment and dementia.[149] As of 2008 there is no concrete evidence that cannabinoids are effective in improving the symptoms of AD or dementia.[150] Some research in its early stages however looks promising.[151]
The cause of Alzheimer's disease is poorly understood.[1] About 70% of the risk is believed to be genetic with many genes usually involved.[6] Other risk factors include a history of head injuries, depression, or hypertension.[1] The disease process is associated with plaques and tangles in the brain.[6] A probable diagnosis is based on the history of the illness and cognitive testing with medical imaging and blood tests to rule out other possible causes.[7] Initial symptoms are often mistaken for normal ageing.[1] Examination of brain tissue is needed for a definite diagnosis.[6] Mental and physical exercise, and avoiding obesity may decrease the risk of AD.[6] There are no medications or supplements that decrease risk.[8]
No treatments stop or reverse its progression, though some may temporarily improve symptoms.[2] Affected people increasingly rely on others for assistance, often placing a burden on the caregiver; the pressures can include social, psychological, physical, and economic elements.[9] Exercise programmes are beneficial with respect to activities of daily living and can potentially improve outcomes.[10] Treatment of behavioural problems or psychosis due to dementia with antipsychotics is common but not usually recommended due to there often being little benefit and an increased risk of early death.[11][12]
In 2015, there were approximately 48 million people worldwide with AD.[2] It most often begins in people over 65 years of age, although 4% to 5% of cases are early-onset Alzheimer's which begin before this.[13] It affects about 6% of people 65 years and older.[1] In 2010, dementia resulted in about 486,000 deaths.[14] It was first described by, and later named after, German psychiatrist and pathologist Alois Alzheimer in 1906.[15] In developed countries, AD is one of the most financially costly diseases.[16][17]
Prevention
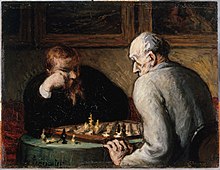
Intellectual activities such as playing chess
or regular social interaction have been linked to a reduced risk of AD
in epidemiological studies, although no causal relationship has been
found.
Medication
Although cardiovascular risk factors, such as hypercholesterolaemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and course of AD,[119][120] statins, which are cholesterol lowering drugs, have not been effective in preventing or improving the course of the disease.[121][122][123]Long-term usage of non-steroidal anti-inflammatory drugs (NSAIDs) is associated with a reduced likelihood of developing AD.[124] Evidence also support the notion that NSAIDs can reduce inflammation related to amyloid plaques.[124] No prevention trial has been completed.[124] They do not appear to be useful as a treatment.[125] Hormone replacement therapy, although previously used, may increase the risk of dementia.[126]
Lifestyle
People who engage in intellectual activities such as reading, playing board games, completing crossword puzzles, playing musical instruments, or regular social interaction show a reduced risk for Alzheimer's disease.[127] This is compatible with the cognitive reserve theory, which states that some life experiences result in more efficient neural functioning providing the individual a cognitive reserve that delays the onset of dementia manifestations.[127] Education delays the onset of AD syndrome, but is not related to earlier death after diagnosis.[128] Learning a second language even later in life seems to delay getting Alzheimer disease.[129] Physical activity is also associated with a reduced risk of AD.[128]Diet
People who eat a healthy, Japanese, or Mediterranean diet have a lower risk of AD.[130] A Mediterranean diet may improve outcomes in those with the disease.[131] Those who eat a diet high in saturated fats and simple carbohydrates (mono- and disaccharide) have a higher risk.[132] The mediterranean diet's beneficial cardiovascular effect has been proposed as the mechanism of action.[133]Conclusions on dietary components have at times been difficult to ascertain as results have differed between population-based studies and randomised controlled trials.[130] There is limited evidence that light to moderate use of alcohol, particularly red wine, is associated with lower risk of AD.[134] There is tentative evidence that caffeine may be protective.[135] A number of foods high in flavonoids such as cocoa, red wine, and tea may decrease the risk of AD.[136][137]
Reviews on the use of vitamins and minerals have not found enough consistent evidence to recommend them. This includes vitamin A,[138][139] C,[140][141] E,[141][142] selenium,[143] zinc,[144] and folic acid with or without vitamin B12.[145] Additionally vitamin E is associated with health risks.[141] Trials examining folic acid (B9) and other B vitamins failed to show any significant association with cognitive decline.[146] In those already affected with AD adding docosahexaenoic acid, an omega-3 fatty acid, to the diet has not been found to slow decline.[147]
Curcumin as of 2010 has not shown benefit in people even though there is tentative evidence in animals.[148] There is inconsistent and unconvincing evidence that ginkgo has any positive effect on cognitive impairment and dementia.[149] As of 2008 there is no concrete evidence that cannabinoids are effective in improving the symptoms of AD or dementia.[150] Some research in its early stages however looks promising.[151]
Friday, 25 March 2016
Heart cancer
Heart cancer is an extremely rare form of cancer that is divided into primary tumors of the heart and secondary tumors of the heart.
Primary malignant cardiac tumors (PMCTs) are even more rare. A study using the Surveillance, Epidemiology and End-Results (SEER) Cancer Registry from 1973-2011 found 551 case of PMCTs, with an incidence of 34 cases per million persons. The study also found that the incidence has doubled over the past 4 decades. The associated mortality was very high, with only 46% of patients are alive by 1 year. Sarcomas and Mesotheliomas had the worst survival, while lymphomas had better survival. When compared with extracardiac tumors, PMCTs had worse survival. [3]
Primary
Most heart tumors begin with myxomas, fibromas, rhabdomyomas, and hamartomas, although malignant sarcomas (such as angiosarcoma or cardiac sarcoma) have been known to occur. In a study of 12,487 autopsies performed in Hong Kong seven cardiac tumors were found, most of which were benign.[1] According to Mayo Clinic: "At Mayo Clinic, on average only one case of heart cancer is seen each year."[1] In a study conducted in the Hospital of the Medical University of Vienna 113 primary cardiac tumour cases were identified in a time period of 15 years with 11 being malignant. The mean survival in the latter group of patients was found to be 26.2 ± 9.8 months.[2]Primary malignant cardiac tumors (PMCTs) are even more rare. A study using the Surveillance, Epidemiology and End-Results (SEER) Cancer Registry from 1973-2011 found 551 case of PMCTs, with an incidence of 34 cases per million persons. The study also found that the incidence has doubled over the past 4 decades. The associated mortality was very high, with only 46% of patients are alive by 1 year. Sarcomas and Mesotheliomas had the worst survival, while lymphomas had better survival. When compared with extracardiac tumors, PMCTs had worse survival. [3]
Atrial myxoma
An atrial myxoma is a benign tumor of the heart, commonly found within the left and right atria on the interatrial septum.
The tumor is derived from multipotential mesenchymal cells and may cause a ball valve-type obstruction.
About 75% of myxomas occur in the left atrium of the heart, usually beginning in the wall that divides the two upper chambers of the heart. The rest are in the right atrium. Right atrial myxomas are sometimes associated with tricuspid stenosis and atrial fibrillation.
Myxomas are more common in women. About 10% of myxomas are passed down through families (inherited). Such tumors are called familial myxomas. They tend to occur in more than one part of the heart at a time, and often cause symptoms at a younger age than other myxomas.
Right atrial myxomas rarely produce symptoms until they have grown to be at least 13 cm (about 5 inches) wide.
Tests may include:
Myxomas may come back if surgery did not remove all of the tumor cells.
Although a myxoma is not cancer, complications are common. Untreated, a myxoma can lead to an embolism (tumor cells breaking off and traveling with the bloodstream), which can block blood flow. Myxoma fragments can move to the brain, eye, or limbs.
If the tumor grows inside the heart, it can block blood flow through the mitral valve and cause symptoms of mitral stenosis. This may require emergency surgery to prevent sudden death.
Causes
Myxomas are the most common type of primary heart tumor.[1]The tumor is derived from multipotential mesenchymal cells and may cause a ball valve-type obstruction.
About 75% of myxomas occur in the left atrium of the heart, usually beginning in the wall that divides the two upper chambers of the heart. The rest are in the right atrium. Right atrial myxomas are sometimes associated with tricuspid stenosis and atrial fibrillation.
Myxomas are more common in women. About 10% of myxomas are passed down through families (inherited). Such tumors are called familial myxomas. They tend to occur in more than one part of the heart at a time, and often cause symptoms at a younger age than other myxomas.
Symptoms
Symptoms may occur at any time, but most often they accompany a change of body position. Symptoms may include:- Shortness of breath with activity
- Platypnea - Difficulty breathing in the upright position with relief in the supine position
- Paroxysmal nocturnal dyspnea - Breathing difficulty when asleep
- Dizziness
- Fainting
- Palpitations - Sensation of feeling your heart beat
- Chest pain or tightness
- Sudden Death (In which case the disease is an autopsy finding)
- Cough
- Fever
- Cachexia - Involuntary weight loss
- General discomfort (malaise)
- Joint pain
- Blue discoloration of the skin, especially the fingers (Raynaud's phenomenon)
- Fingers that change color upon pressure or with cold or stress
- Clubbing - Curvature of nails accompanied with soft tissue enlargement of the fingers
- Swelling - any part of the body
- Presystolic heart murmur[2]
Diagnosis
A doctor will listen to the heart with stethoscope. A "tumor plop" (a sound related to movement of the tumor), abnormal heart sounds, or a murmur similar to the mid-diastolic rumble of mitral stenosis may be heard. These sounds may change when the patient changes position.
Echocardiogram of Atrial myxoma
Tests may include:
- Echocardiogram and Doppler study
- Chest x-ray
- CT scan of chest
- Heart MRI
- Left heart angiography
- Right heart angiography
- ECG—may show atrial fibrillation
Treatment
The tumor must be surgically removed. Some patients will also need their mitral valve replaced. This can be done during the same surgery.Myxomas may come back if surgery did not remove all of the tumor cells.
Prognosis
An embolized fragment of an atrial myxoma in the iliac bifurcation.
If the tumor grows inside the heart, it can block blood flow through the mitral valve and cause symptoms of mitral stenosis. This may require emergency surgery to prevent sudden death.
Mediastinal tumor
The mediastinum is the cavity that separates the lungs from the rest of the chest. It contains the heart, esophagus, trachea, thymus, and aorta. The mediastinum has three main parts: the anterior mediastinum (front), the middle mediastinum, and the posterior mediastinum (back).
The most common mediastinal masses are neurogenic tumors (20% of mediastinal tumors), usually found in the posterior mediastinum, followed by thymoma (15-20%) located in the anterior mediastinum.[1]
Masses in the anterior portion of the mediastinum can include thymoma, lymphoma, pheochromocytoma, germ cell tumors including teratoma, thyroid tissue, and parathyroid lesions. Masses in this area are more likely to be malignant than those in other compartments.[2][3]
Masses in the posterior portion of the mediastinum tend to be neurogenic in origin, and in adults tend to be of neural sheath origin including neurilemomas and neurofibromas.[1]
Lung cancer typically spreads to the lymph nodes in the mediastinum.
In several editions of Physical Diagnosis,[4] concerning mediastinal tumors the author writes:
The most common mediastinal masses are neurogenic tumors (20% of mediastinal tumors), usually found in the posterior mediastinum, followed by thymoma (15-20%) located in the anterior mediastinum.[1]
Masses in the anterior portion of the mediastinum can include thymoma, lymphoma, pheochromocytoma, germ cell tumors including teratoma, thyroid tissue, and parathyroid lesions. Masses in this area are more likely to be malignant than those in other compartments.[2][3]
Masses in the posterior portion of the mediastinum tend to be neurogenic in origin, and in adults tend to be of neural sheath origin including neurilemomas and neurofibromas.[1]
Lung cancer typically spreads to the lymph nodes in the mediastinum.
In several editions of Physical Diagnosis,[4] concerning mediastinal tumors the author writes:
Diagnosis
According to Christian1 the mediastinal neoplasms which are neither so rare nor so obscure as to make diagnosis practically impossible are: (1) Sarcoma (including lymphosarcoma, leucaemic growths, and Hodgkins' disease; (2) Teratoma and cyst.
Thursday, 24 March 2016
Borderline personality disorder
Borderline personality disorder (BPD) is a pattern of abnormal behavior characterized by impulsivity, unstable affect, inconsistent interpersonal relationships, and poor self-image. Some individuals also display uncontrollable anger and depression. The pattern is typically present by early adulthood, and occurs across a variety of situations and contexts.[3] Other symptoms include intense fears of abandonment, sensitivity to feelings of rejection, and irritability of vague or uncertain origin.[3][4] People with BPD often engage in idealization and devaluation of others, alternating between high positive regard and great disappointment.[5] Self-harm, suicidal behavior, and substance abuse are commonly associated.[6]
The cause of BPD is unclear but believed to involve both genetic and environmental factors. A study done on twins suggested the illness could be inherited. Traits such as impulsiveness and aggression can be attributed to temperament.[7] There is evidence that abnormalities of the frontolimbic networks are associated with many of the symptoms.[8] The disorder is recognized in the Diagnostic and Statistical Manual of Mental Disorders. Since a personality disorder is a pervasive, enduring, and inflexible pattern of maladaptive inner experiences and pathological behavior, there is a general reluctance to diagnose personality disorders before adolescence or early adulthood.[9] However, some practitioners emphasize that without early treatment, the symptoms may worsen.[10]
There is an ongoing debate about the terminology of this disorder, especially the suitability of the word "borderline".[11][12] The ICD-10 manual refers to the disorder as emotionally unstable personality disorder and has similar diagnostic criteria. In the DSM-5, the name of the disorder remains the same as in the previous editions
The cause of BPD is unclear but believed to involve both genetic and environmental factors. A study done on twins suggested the illness could be inherited. Traits such as impulsiveness and aggression can be attributed to temperament.[7] There is evidence that abnormalities of the frontolimbic networks are associated with many of the symptoms.[8] The disorder is recognized in the Diagnostic and Statistical Manual of Mental Disorders. Since a personality disorder is a pervasive, enduring, and inflexible pattern of maladaptive inner experiences and pathological behavior, there is a general reluctance to diagnose personality disorders before adolescence or early adulthood.[9] However, some practitioners emphasize that without early treatment, the symptoms may worsen.[10]
There is an ongoing debate about the terminology of this disorder, especially the suitability of the word "borderline".[11][12] The ICD-10 manual refers to the disorder as emotionally unstable personality disorder and has similar diagnostic criteria. In the DSM-5, the name of the disorder remains the same as in the previous editions
Wednesday, 23 March 2016
anorexia
Anorexia nervosa, often referred to simply as anorexia,[1] is an eating disorder characterized by a low weight, fear of gaining weight, a strong desire to be thin, and food restriction.[2] Many people with anorexia see themselves as overweight even though they are underweight.[2][3] If asked they usually deny they have a problem with low weight.[4]
Often they weigh themselves frequently, eat only small amounts, and
only eat certain foods. Some will exercise excessively, force themselves
to vomit, or use laxatives to produce weight loss. Complications may include osteoporosis, infertility and heart damage, among others.[2] Women will often stop having menstrual periods.[4]
The cause is not known. There appear to be some genetic components with identical twins more often affected than non-identical twins.[3] Cultural factors also appear to play a role with societies that value thinness having higher rates of disease.[4] Additionally, it occurs more commonly among those involved in activities that value thinness such as high level athletics, modelling, and dancing.[4][5] Anorexia often begins following a major life change or stress inducing event. The diagnosis requires a significantly low weight. The severity of disease is based on body mass index (BMI) in adults with mild disease having a BMI of greater than 17, moderate a BMI of 16 to 17, severe a BMI of 15 to 16, and extreme a BMI less than 15. In children a BMI for age percentile of less than the 5th percentile is often used.[4]
Treatment of anorexia involves restoring a healthy weight, treating the underlying psychological problems, and addressing behaviors that promote the problem. While medications do not help with weight gain, they may be used to help with associated anxiety or depression.[2] A number of types of therapy may be useful including an approach where parents assume responsibility for feeding their child, known as Maudsley family therapy and cognitive behavioral therapy.[2][6] Sometimes people require admission to hospital to restore weight.[7] Evidence for benefit from nasogastric tube feeding; however, is unclear.[8] Some people will just have a single episode and recover while others may have many episodes over years.[7] Many complications improve or resolve with regaining of weight.[7]
Globally anorexia is estimated to affect two million people as of 2013.[9] It is estimated to occur in 0.9% to 4.3% of women and 0.2% to 0.3% of men in Western countries at some point in their life.[10] About 0.4% of young females are affected in a given year and it is estimated to occur ten times less commonly in males.[4][10] Rates in most of the developing world are unclear.[4] Often it begins during the teen years or young adulthood.[2] While anorexia became more commonly diagnosed during the 20th century it is unclear if this was due to an increase in its frequency or simply better diagnosis.[3] In 2013 it directly resulted in about 600 deaths globally up from 400 deaths in 1990.[11] Eating disorders also increase a person's risk of death from a wide range of other causes including suicide.[2][10] About 5% of people with anorexia die from complications over a ten-year period.[4] The term anorexia nervosa was first used in 1873 by William Gull to describe this condition
The cause is not known. There appear to be some genetic components with identical twins more often affected than non-identical twins.[3] Cultural factors also appear to play a role with societies that value thinness having higher rates of disease.[4] Additionally, it occurs more commonly among those involved in activities that value thinness such as high level athletics, modelling, and dancing.[4][5] Anorexia often begins following a major life change or stress inducing event. The diagnosis requires a significantly low weight. The severity of disease is based on body mass index (BMI) in adults with mild disease having a BMI of greater than 17, moderate a BMI of 16 to 17, severe a BMI of 15 to 16, and extreme a BMI less than 15. In children a BMI for age percentile of less than the 5th percentile is often used.[4]
Treatment of anorexia involves restoring a healthy weight, treating the underlying psychological problems, and addressing behaviors that promote the problem. While medications do not help with weight gain, they may be used to help with associated anxiety or depression.[2] A number of types of therapy may be useful including an approach where parents assume responsibility for feeding their child, known as Maudsley family therapy and cognitive behavioral therapy.[2][6] Sometimes people require admission to hospital to restore weight.[7] Evidence for benefit from nasogastric tube feeding; however, is unclear.[8] Some people will just have a single episode and recover while others may have many episodes over years.[7] Many complications improve or resolve with regaining of weight.[7]
Globally anorexia is estimated to affect two million people as of 2013.[9] It is estimated to occur in 0.9% to 4.3% of women and 0.2% to 0.3% of men in Western countries at some point in their life.[10] About 0.4% of young females are affected in a given year and it is estimated to occur ten times less commonly in males.[4][10] Rates in most of the developing world are unclear.[4] Often it begins during the teen years or young adulthood.[2] While anorexia became more commonly diagnosed during the 20th century it is unclear if this was due to an increase in its frequency or simply better diagnosis.[3] In 2013 it directly resulted in about 600 deaths globally up from 400 deaths in 1990.[11] Eating disorders also increase a person's risk of death from a wide range of other causes including suicide.[2][10] About 5% of people with anorexia die from complications over a ten-year period.[4] The term anorexia nervosa was first used in 1873 by William Gull to describe this condition
prostate cancer
Early prostate cancer usually has no clear symptoms. Sometimes,
however, prostate cancer does cause symptoms, often similar to those of
diseases such as benign prostatic hyperplasia. These include frequent urination, nocturia (increased urination at night), difficulty starting and maintaining a steady stream of urine, hematuria (blood in the urine), and dysuria
(painful urination). A study based on the 1998 Patient Care Evaluation
in the US found that about a third of patients diagnosed with prostate
cancer had one or more such symptoms, while two thirds had no symptoms.[13]
Prostate cancer is associated with urinary dysfunction as the prostate gland surrounds the prostatic urethra. Changes within the gland, therefore, directly affect urinary function. Because the vas deferens deposits seminal fluid into the prostatic urethra, and secretions from the prostate gland itself are included in semen content, prostate cancer may also cause problems with sexual function and performance, such as difficulty achieving erection or painful ejaculation.[13]
Advanced prostate cancer can spread to other parts of the body, possibly causing additional symptoms. The most common symptom is bone pain, often in the vertebrae (bones of the spine), pelvis, or ribs. Spread of cancer into other bones such as the femur is usually to the proximal or nearby part of the bone. Prostate cancer in the spine can also compress the spinal cord, causing tingling, leg weakness and urinary and fecal incontinence.[14]
No single gene is responsible for prostate cancer; many different genes have been implicated. Mutations in BRCA1 and BRCA2, important risk factors for ovarian cancer and breast cancer in women, have also been implicated in prostate cancer.[27] Other linked genes include the Hereditary Prostate cancer gene 1 (HPC1), the androgen receptor, and the vitamin D receptor.[24] TMPRSS2-ETS gene family fusion, specifically TMPRSS2-ERG or TMPRSS2-ETV1/4 promotes cancer cell growth.[28]
Two large genome-wide association studies linking single nucleotide polymorphisms (SNPs) to prostate cancer were published in 2008.[29][30] These studies identified several SNPs which substantially affect the risk of prostate cancer. For example, individuals with TT allele pair at SNP rs10993994 were reported to be at 1.6 times higher risk of prostate cancer than those with the CC allele pair. This SNP explains part of the increased prostate cancer risk of African American men as compared to American men of European descent, since the C allele is much more prevalent in the latter; this SNP is located in the promoter region of the MSMB gene, thus affects the amount of MSMB protein synthesized and secreted by epithelial cells of the prostate.[31]
Lower blood levels of vitamin D may increase the risk of developing prostate cancer.[36]
Folic acid supplements have no effect on the risk of developing prostate cancer.[37]
Infection or inflammation of the prostate (prostatitis) may increase the chance for prostate cancer while another study shows infection may help prevent prostate cancer by increasing blood to the area. In particular, infection with the sexually transmitted infections chlamydia, gonorrhea, or syphilis seems to increase risk.[40] Finally, obesity[41] and elevated blood levels of testosterone[42] may increase the risk for prostate cancer. There is an association between vasectomy and prostate cancer; however, more research is needed to determine if this is a causative relationship.[43]
Research released in May 2007, found that US war veterans who had been exposed to Agent Orange had a 48% increased risk of prostate cancer recurrence following surgery.[44]
In 2006, a previously unknown retrovirus, Xenotropic MuLV-related virus or XMRV, was associated with human prostate tumors,[45] but subsequent reports on the virus were contradictory,[46][47] and the original 2006 finding was instead due to a previously undetected contamination.[48] The journals Science and PlosONE both retracted XMRV related articles.[49][50]
While the available evidence is weak,[54] tentative results suggest that frequent ejaculation may decrease the risk of prostate cancer.[55] A study, over eight years, showed that those that ejaculated most frequently (over 21 times per month on average) were less likely to get prostate cancer.[56] The results were broadly similar to the findings of a smaller Australian study.[57]
Prostate cancer is associated with urinary dysfunction as the prostate gland surrounds the prostatic urethra. Changes within the gland, therefore, directly affect urinary function. Because the vas deferens deposits seminal fluid into the prostatic urethra, and secretions from the prostate gland itself are included in semen content, prostate cancer may also cause problems with sexual function and performance, such as difficulty achieving erection or painful ejaculation.[13]
Advanced prostate cancer can spread to other parts of the body, possibly causing additional symptoms. The most common symptom is bone pain, often in the vertebrae (bones of the spine), pelvis, or ribs. Spread of cancer into other bones such as the femur is usually to the proximal or nearby part of the bone. Prostate cancer in the spine can also compress the spinal cord, causing tingling, leg weakness and urinary and fecal incontinence.[14]
Risk factors
A complete understanding of the causes of prostate cancer remains elusive.[15] The primary risk factors are obesity, age and family history. Prostate cancer is very uncommon in men younger than 45, but becomes more common with advancing age. The average age at the time of diagnosis is 70.[16] However, many men never know they have prostate cancer. Autopsy studies of Chinese, German, Israeli, Jamaican, Swedish, and Ugandan men who died of other causes have found prostate cancer in 30% of men in their 50s, and in 80% of men in their 70s.[17] Men who have first-degree family members with prostate cancer appear to have double the risk of getting the disease compared to men without prostate cancer in the family.[18] This risk appears to be greater for men with an affected brother than for men with an affected father. In the United States in 2005, there were an estimated 230,000 new cases of prostate cancer and 30,000 deaths due to prostate cancer.[19] Men with high blood pressure are more likely to develop prostate cancer.[20] There is a small increased risk of prostate cancer associated with lack of exercise.[21] A 2010 study found that prostate basal cells were the most common site of origin for prostate cancers.[22]Genetic
Genetic background may contribute to prostate cancer risk, as suggested by associations with race, family, and specific gene variants. Men who have a first-degree relative (father or brother) with prostate cancer have twice the risk of developing prostate cancer, and those with two first-degree relatives affected have a fivefold greater risk compared with men with no family history.[23] In the United States, prostate cancer more commonly affects black men than white or Hispanic men, and is also more deadly in black men.[24][25] In contrast, the incidence and mortality rates for Hispanic men are one third lower than for non-Hispanic whites. Studies of twins in Scandinavia suggest that 40% of prostate cancer risk can be explained by inherited factors.[26]No single gene is responsible for prostate cancer; many different genes have been implicated. Mutations in BRCA1 and BRCA2, important risk factors for ovarian cancer and breast cancer in women, have also been implicated in prostate cancer.[27] Other linked genes include the Hereditary Prostate cancer gene 1 (HPC1), the androgen receptor, and the vitamin D receptor.[24] TMPRSS2-ETS gene family fusion, specifically TMPRSS2-ERG or TMPRSS2-ETV1/4 promotes cancer cell growth.[28]
Two large genome-wide association studies linking single nucleotide polymorphisms (SNPs) to prostate cancer were published in 2008.[29][30] These studies identified several SNPs which substantially affect the risk of prostate cancer. For example, individuals with TT allele pair at SNP rs10993994 were reported to be at 1.6 times higher risk of prostate cancer than those with the CC allele pair. This SNP explains part of the increased prostate cancer risk of African American men as compared to American men of European descent, since the C allele is much more prevalent in the latter; this SNP is located in the promoter region of the MSMB gene, thus affects the amount of MSMB protein synthesized and secreted by epithelial cells of the prostate.[31]
Dietary
While some dietary factors have been associated with prostate cancer the evidence is still tentative.[32] Evidence supports little role for dietary fruits and vegetables in prostate cancer occurrence.[33] Red meat and processed meat also appear to have little effect in human studies.[34] Higher meat consumption has been associated with a higher risk in some studies.[35]Lower blood levels of vitamin D may increase the risk of developing prostate cancer.[36]
Folic acid supplements have no effect on the risk of developing prostate cancer.[37]
Medication exposure
There are also some links between prostate cancer and medications, medical procedures, and medical conditions.[38] Use of the cholesterol-lowering drugs known as the statins may also decrease prostate cancer risk.[39]Infection or inflammation of the prostate (prostatitis) may increase the chance for prostate cancer while another study shows infection may help prevent prostate cancer by increasing blood to the area. In particular, infection with the sexually transmitted infections chlamydia, gonorrhea, or syphilis seems to increase risk.[40] Finally, obesity[41] and elevated blood levels of testosterone[42] may increase the risk for prostate cancer. There is an association between vasectomy and prostate cancer; however, more research is needed to determine if this is a causative relationship.[43]
Research released in May 2007, found that US war veterans who had been exposed to Agent Orange had a 48% increased risk of prostate cancer recurrence following surgery.[44]
Infectious disease
An association with gonorrhea has been found, but a mechanism for this relationship has not been identified.[6]In 2006, a previously unknown retrovirus, Xenotropic MuLV-related virus or XMRV, was associated with human prostate tumors,[45] but subsequent reports on the virus were contradictory,[46][47] and the original 2006 finding was instead due to a previously undetected contamination.[48] The journals Science and PlosONE both retracted XMRV related articles.[49][50]
Sexual factors
Several case-control studies have shown that having many lifetime sexual partners or starting sexual activity early in life substantially increases the risk of prostate cancer.[51][52][53]While the available evidence is weak,[54] tentative results suggest that frequent ejaculation may decrease the risk of prostate cancer.[55] A study, over eight years, showed that those that ejaculated most frequently (over 21 times per month on average) were less likely to get prostate cancer.[56] The results were broadly similar to the findings of a smaller Australian study.[57]
Subscribe to:
Comments
(
Atom
)